CASE REPORT / OLGU SUNUMU
Doi: 10.5798/diclemedj.0921.2012.01.0108
Approach to hypersplenism due to splenic metastasis of breast cancer: A
case report
Meme kanseri dalak metastazına bağlı gelişen hipersplenizme
yaklaşım: Olgu sunumu
Mehmet
Küçüköner1, M. Ali Kaplan1, Ali İnal1,
Abdurrahman Işıkdoğan1, Uğur Fırat2, Akın Önder3,
Feyzullah Uçmak4, Hakan Önder5, M. Recai Akdoğan6
1Dicle University Medical
Faculty, Department of Medical Oncology Diyarbakir, Turkey
2Dicle University Medical Faculty,
Department s of Pathology Diyarbakir, Turkey
3Dicle University Medical Faculty,
Department of General Surgery Diyarbakir, Turkey
4Dicle University Medical Faculty,
Department of Gastroenterology Diyarbakir, Turkey
5Dicle University Medical
Faculty, Department ns of Radiology Diyarbakir, Turkey
6Dicle University Medical
Faculty, Department of Internal Medicine Diyarbakir, Turkey
Yazışma Adresi /Correspondence: Dr.
Mehmet Küçüköner, Dicle University, Medicine Faculty, Dept. Medical Oncology,
Diyarbakir, Turkey
Email: drmehmetonko@hotmail.com
Geliş Tarihi / Received: 06.08.2011, Kabul Tarihi /
Accepted: 23.12.2011
ABSTRACT
The most common sites for
breast cancer metastasis include the bones, lungs, liver, lymph nodes, and
brain. However, splenic metastasis of breast cancer is extremely rare.
Hypersplenism occurs as a cause of severe hemolytic anemia in carcinomas or
with marked splenic enlargement related to splenic metastasis. We presented a
rare case of breast cancer with splenic metastasis that was undergone
splenectomy to correct cytopenia related to hypersplenism. In the light of this
case, splenectomy can be beneficial in the patients with hypersplenism.
Key words: Breast cancer, hypersplenism,
splenectomy.
ÖZET
Meme
kanserinin en sık metastaz bölgeleri kemikler, akciğerler, karaciğer, lenf
nodları ve beyindir. Meme kanserinin dalağa metastazı ise çok nadirdir.
Hipersplenizm, karsinomalarda ciddi hemolitik aneminin bir nedeni olarak veya
dalak metastazına bağlı aşırı dalak büyümesiyle ortaya çıkar. Hipersplenizme
bağlı pansitopeninin tedavisinde splenektomi yararlı olabilmektedir. Biz
hipersplenizm ile ilişkili sitopeniyi düzeltmek için splenektomi yapılan dalak
metastazlı nadir bir meme kanseri olgusunu sunduk. Bu olgunun ışığında
metastatik kanserli hastalarda dalak metastazına bağlı oluşan hipersplenizm
tedavisinde splenektomi faydalı olabilmektedir.
Anahtar
kelimeler: Meme
kanseri, hipersplenizm, splenektomi.
INTRODUCTION
Metastatic tumors of the
spleen are rare and usually occur in the presence of disseminated visceral
metastases. The most common tumors causing splenic metastases are breast, lung,
colorectal, and ovarian carcinoma and melanoma.1 Hypersplenism
represents the increased pooling and/or destruction of the corpuscular elements
of the blood by the enlarged spleen. Hypersplenism is a condition which
cytopenia develop due to splenomegaly and may be suspected as a cause of severe
hemolytic anemia in advanced neoplasms.2 Splenectomy can be
performed as palliation with acceptable morbidity in patients with symptomatic
splenomegaly to improve the quality of life.1 In cases of isolated
splenic metastasis, especially in colon and breast cancer, splenectomy is
beneficial because it has a low complication rate and potential long term
survival is higher.2,3 In the literature, hypersplenism due to
splenic metastasis of breast cancer is very rare. We report herein a rare case
of a splenic metastasis due to breast cancer in a young patient who underwent
splenectomy for the correction of cytopenia as a cause of hypersplenism.
CASE REPORT
A 33-year old premenopausal
patient presented with left breast mass. She was diagnosed with invasive ductal
carcinoma by biopsy. On the first examination of the patient, ECOG performance
score was 1 and breast examination revealed an 8×4 cm mass in the left breast.
Abdominal examination revealed hepatomegaly. Other system examinations were
normal. Hematological analysis was normal except anemia (hemoglobin: 10g/dl).
Biochemical parameters including liver function tests and renal function tests
were within normal limits.
Computed tomography of the abdomen and thorax revealed
multiple hipodens lesions in the liver and a mass in the left breast. Additionally,
bone sintigraphy of the patient presented bone metastasis. In these images, the
spleen size was in normal range. The clinical and radiological TNM staging was
T4N2M1. The pathological biopsy revealed estrogen and progesterone receptor
(+), and cERB2 (-). Palliative chemotherapy was administered; three cycles of
cyclophosphamide, doxorubicin, and bisphosphonate. Three months after the
chemotheraphy, thrombocytopenia (platelet range: 60.000-80.000) occurred. Since
the platelet counts had not increased, bone marrow biopsy was performed. The
bone marrow biopsy documented an increased cellularity and carcinoma
infiltration. Although there was a thrombocytopenia, chemotherapy (weekly
paclitaxel and capesitabine) was administered due to the disease progression.
Because of thrombocytopenia of the patient, lower
doses of myelosupressive adverse chemotherapeutics were administered as
monotherapy. Firstly, paclitaxel was given to the patient every week during 6
months. When chemotherapy response decreased, oral capesitabine was
administered nearly for 6 months. The disease was stable as clinically and
radiologically nearly 16 months from the diagnosis. The patient exhibited a
partial response to chemotherapy for nearly 16 months. In the course of this
time, platelet count range was 20.000-60.000. Due to decrease platelet counts
below 20.000, and gingival bleeding and conjunctival hemorrhage, the patient
was hospitalized. Abdominal examination revealed hepatomegaly and a new
occurrence of splenomegaly.
In the computary tomography, multiple metastasis and
organomegali presented in the spleen and liver (Figure 1). The laboratory
results were as follows; hemogram: White blood cell: 2940 K/UL, Neutrophil:
1620K/UL, Hemoglobin:8 gr/dl, Hematocrit:%24, and Platelets:17200K/UL.
Additionally, the blood biochemical analysis was normal. Direct and indirect
Coombs tests were negative. Although the patient was given steroid and medical
therapy, platelet level was continued as 5.000-20.000. Because of the gingival
and conjunctival bleeding due to thrombocytopenia, the patient was given
frequent thrombocyte and erythrocyte transfusions once in two days for a month.
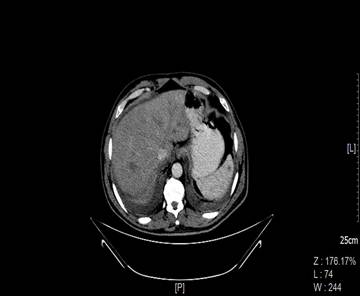
Figure 1. Multiple metastasis and organomegali presented in the spleen and liver
In the computed tomography
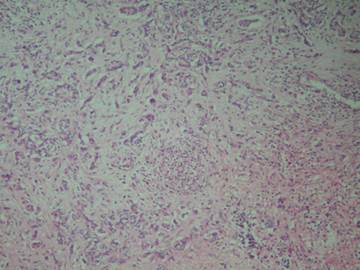
Figure 2. Malignant Epithelial Tumor infiltration in a desmoplastic stroma in the
spleen. (H&EstainX100).
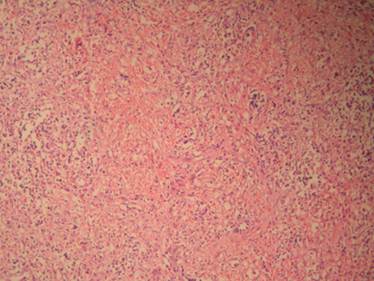
Figure
Pancytopenia related to hypersplenism was considered
because of the increased cellularity documented in bone marrow biopsy, and
splenomegaly demonstrated in the ultrasonography. The patient was consulted to
surgery for splenectomy because of thrombocyte was not improved with medical
therapy. After preoperative preparation of the patient with platelet
transfusions, splenectomy was performed. Two days after splenectomy, the
platelet level of the patient increased to 182.000. Adenocarcinoma metastasis
was reported after splenectomy material had been evaluated. The diagnosis report
was as follows; Malignant Epithelial Tumor infiltration in a desmoplastic
stroma in the spleen (Figure2, 3 H&EstainX100). In the examination of
immunohistochemical, cERB2 was negative. After the splenectomy, the patient has
been followed up with normal platelet level for nearly 9 months. Afterwards,
palliative chemotherapy was applied to the patient again. The disease of breast
cancer of the patient has continued without any progression. Platelet count was
122.000 K/UL during the last chemotherapy. However, myelosuppresion and hepatic
toxicity developed after chemotherapy and unfortunately the patient passed
away.
DISCUSSION
Metastatic tumors of the
spleen are rare and usually occur in the presence of disseminated visceral
metastases at terminal stage. The prevalence of splenic metastases in large
populations with cancer was mainly obtained from autopsy series ranged between
2.3% and 7.1%.4 In a Japanese study, in 0.15% of the patients, splenic
metastasis was detected by ultrasonography.5 The rarity of splenic metastases
could be explained by anatomic factors and the inhibitory effect of the splenic
microenvironment on the growth of metastatic cells. Several theories have been
showed efforts to the resistance of spleen parenchyma against metastases. Some of
these include the ability of the splenic capsule to form a physical barrier,
angled and a corrugated anatomic feature of splenic artery and immunological
defense of the spleen against neoplastic cells.6
Hypersplenism represents the increased pooling and/or
destruction of the corpuscular elements of the blood by the enlarged spleen.
Hypersplenism may be suspected as a cause of severe hemolytic anemia in
advanced carcinoma. Hypersplenism was diagnosed in connection with
splenomegaly, pancytopenia and increased cellularity documented in bone marrow
biopsy. Immune mechanisms and splenomegaly are responsible for hypersplenism.7,8
For these reasons, our patient was given steroid and medical therapy. Since the
response had not been achieved for the medical therapy, due to low thrombocyte
count, splenectomy was performed. After splenectomy, the patient has been
followed up with normal platelet level for nearly 9 months. The disease of
breast cancer of the patient has continued without progression during these
nine months of period. At the tenth months, the patient passed away because of
the toxicity of chemotherapy in the 10th months.
In the literature, two cases have been reported that
hypersplenism was corrected with splenectomy in patients with advanced breast
cancer who did not response to medical therapy. Additionally, splenectomy which
was performed to the patient with isolated splenic metastasis has improved
overall survival. Splenic metastasis in ovarian carcinomas has been reported in
the literature and splenectomy has been shown to be beneficial for these
patients. Splenectomy is meaningful to the isolated spleen metastasis of the
carcinomas. In the literature, it was reported that splenectomy was beneficial
for the patients with over, colon and breast cancer with the spleen metastasis.2,9
Moreover, splenectomy can be performed with palliative purposes in patients
with acceptable morbidity and symptomatic splenomegaly (cytopenia with
hypersplenism).1
We presented a rare case of breast cancer with splenic
metastasis who underwent splenectomy to correct cytopenia related with
hypersplenism. Additionally, in the lights of these cases with hypersplenism in
the literature, splenectomy may be beneficial in patients with hipersplenism.
REFERENCES
1. Comperat E, Bardier-Dupas
A, Camparo P, Capron F, Charlotte F. Splenic metastases: clinicopathologic
presentation, differential diagnosis, and pathogenesis. Arch Pathol Lab Med
2007;131(6):965-9.
2. Dunn MA, Goldwein MI.
Hypersplenism in advanced breast cancer: report of a patient treated with
splenectomy. Cancer 1975;35(5):1449-2.
3. Slavin JD, Mathews J,
Spencer RP. Splenectomy for splenic metastasis from carcinoma colon. Clin Nucl
Med 1986;11(7):491-2.
4. Berge T. Splenic
metastases: frequencies and patterns. Acta Pathol Microbiol Scand.
1974;82:499-6.
5. Ishida H, Konno K, Ishida
J, et al O. Isolated splenic metastases. J Ultrasound Med. 1997;16(11):743-9.
6. Lee SS, Morgenstern L,
Phillips EH, Hiatt JR, Margulies DR. Splenectomy for splenic metastases: a
changing clinical spectrum. Am Surg 2000;66(9):837-0.
7. Baranyay F. Case report:
diffuse splenic metastasis of occult breast cancer with incompatible blood
group antigenic determinants. Acta Histochem 2009;111(4):343-8.
8. Nese Zehra Kavak, Birgul
Karakoc. Pregnancy, primary hypersplenism and portal hypertension. T Klin J
Gynecol Obst 2001;11(2):89-90.
9. Piers A. C. Gatenby,
Satvinder S. Mudan, Andrew C. Wotherspoon. Splenectomy for non-haematological
metastatic malignant disease. Langenbecks Arch Surg 2011 396:625-8.