OLGU SUNUMU / CASE REPORT
Doi: 10.5798/diclemedj.0921.2012.01.0104
Cesarean scar pregnancy treated with methotrexate and
dilatation-currettage: Case report
Metotreksat ve dilatasyon-küretaj ile tedavi edilen
sezeryan skar gebeliği: Olgu sunumu
Deniz Cemgil
Arıkan1, Emre Turgut2, Gürkan Kıran1, Hakan Kıran1
1Sütçü Imam University School
of Medicine, Department of Obstetrics and Gynecology, Kahramanmaras, Turkey
2Istanbul Education and
Research Hospital, Department of Obstetrics and Gynecology, Istanbul, Turkey
Yazışma Adresi
/Correspondence: Dr. Deniz Cemgil Arıkan, Sütçü İmam Üniversitesi
Kadın Hastalıkları ve Doğum AD, Kahramanmaraş, Türkiye
Email: drdenizarikan@hotmail.com
Geliş Tarihi /
Received:16.06.2010, Kabul Tarihi / Accepted: 25.11.2010
ABSTRACT
Cesarean scar pregnancy (CSP)
is the rarest form of ectopic pregnancies that can cause serious complications.
A 37 year-old woman with past history of gravida 4, parity 2, cesarian section,
admitted to our outpatient clinic with the complaint of mild pelvic pain and 6
weeks 2 day of amenorrhea. On admission, her serum β-human chorionic
gonadotropin (β-hCG) level was 26905 mIU/mL and
transvaginal ultrasound revealed a 24 mm gestational sac implanted at the site
of her prior cesarean section scar. Initial treatment with single-dose systemic
methotrexate (MTX) (1mg/kg; 60 mg) was not sufficient so the dose of MTX (60
mg) was repeated. In the follow-up the gestational sac continued to increase in
size and patient started to feel abdominal discomfort, so we performed an
ultrasound-guided dilatation and curettage to obtain complete remission. MTX
treatment alone or in conjunction with dilatation-curettage may avoid
unnecessary laparotomy, hysterectomy and preserve fertility CSP patients.
Key words: Cesarean scar pregnancy,
methotrexate, dilatation and curettage
ÖZET
Sezeryan
skar gebelikleri ektopik gebeliklerin ciddi komplikasyonlara
sebep olabilen en nadir formudur. 37 yaşında, geçmişinde 4 gebelik 4, 2 doğum
2ve bir sezaryen bulunan kadın hasta 6 hafta 2 gündür adet görememe ve hafif
pelvik ağrı şikayetleri ile polikliniğimize başvurdu.
Başvuru anında beta- insan koriyonik gonadotropin (β-hCG) değeri 26905
mIU/mL idi ve transvajinal ultrasonografide önceki sezeryan skarına uyan
bölgeye yerleşmiş 24 mm boyutunda gestasyonal kese izlendi. Başlangıçta
uygulanan tek doz sistemik metotreksat (MTX) (1mg/kg; 60 mg) tedavisi etkili
olmadığı için MTX (60mg) dozu tekrarlandı. Takipte gestasyonal kesenin
boyutları büyümeye devam etti ve hasta karın ağrısı hissetmeye başladı, bu
nedenle komplet remisyon amacıyla ultrason eşliğinde
dilatasyon ve küretaj işlemi uyguladık. Sezeryan skar gebeliklerinde MTX
tedavisi tek başına veya dilatasyon-küretaj işlemi ile birlikte uygulandığında,
gereksiz laparotomi ve histerektomiyi önleyerek fertiliteyi koruyabilir.
Anahtar
kelimeler:
Sezeryan skar gebeliği, metotreksat, dilatasyon-küretaj
INTRODUCTION
Cesarean scar pregnancy (CSP)
is the rarest form of ectopic pregnancies with an incidence of 1:1800-1:2216 in
women with an ectopic pregnancy and at least one previous cesarean section.1
However, with rising cesarean section rates and widespread access to imaging
modalities such as sonography and magnetic resonance imaging (MRI), its
incidence has been rising.1
In CSP, the gestational sac is implanted in the
myometrium at the site of a previous cesarean section. Early diagnosis of CSP
is essential to avoid serious complication such as severe hemorrhage, which may
require hysterectomy and endanger the womans life, and affect negatively on
future fertility.2 Also, clinically stable patients have more
treatment options, including conservative management. Therefore, physicians,
particularly obstetricians/gynecologists and radiologists, should have a
heightened awareness of this serious and potentially fatal pregnancy
complication.
In this case report, we present a CSP in a woman who
wishes to preserve her fertility, and its treatment with the systemic
administration of methotrexate (MTX), and dilatation and curettage.
CASE REPORT
A 37 year-old woman with past
history of gravida 4, parity 2, cesarian section 1, admitted to our outpatient
clinic with the complaint of mild pelvic pain and 6 weeks 2 day of amenorrhea.
Her past obstetrical history included 2 ( 11 years and
9 years ago) previous lower segment cesarean sections. On admission, her serum
β-human chorionic gonadotropin (β-hCG) level was 26905
mIU/mL. Transvaginal ultrasound revealed a 24 mm gestational sac within
a fetus with cardiac activity measuring 5.4 mm (6 weeks 2 days gestation)
implanted at the site of her prior cesarean section scar (Picture 1). A
single-dose MTX (1mg/kg; 60 mg) was administered intramuscularly. The dose of
MTX (60 mg) was repeated on the 4th day of follow up, because the fetal cardiac
activity was still present. Three days later fetal cardiac activity became (-)
and serum β-hCG level was 50287 mIU/mL. We decided to follow-up the
patient and thereafter serum β-hCG levels declined to 46686
mIU/mL and 38785 mIU/mL within 4 days respectively. Fourteen days later
from the second dose of MTX serum β-hCG level declined to 12490 mIU/mL, but gestational sac continued to increase in
size and patient started to feel abdominal discomfort. Therefore, we performed
an ultrasound-guided dilatation and curettage. The operation was uncomplicated
and serum β-hCG level declined to within normal range 56 days after
initiation of the treatment.
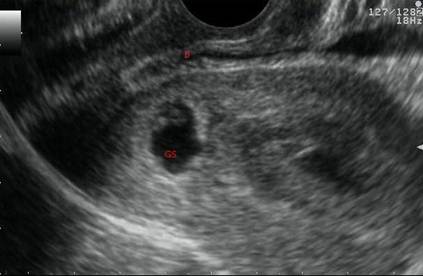
Picture 1: Ultrasound view of cesarean scar pregnancy (B:
bladder; GS: gestational sac)
DISCUSSION
The exact cause of CSP is
still unknown. Several risk factors, including the number of cesarean sections,
the time interval between the previous cesarean section and the subsequent
pregnancy, and the indications for the previous cesarean section have been
suggested, but it is uncertain whether these factors are truly related to CSP.3
As etiology, there is a challenge in treatment of CSP.
Due to the relative rarity of the condition there are no optimal lines for
therapy. Treatment modalities are either medical or surgical; dilatation,
curettage and excision of trophoblastic tissues using laparotomy or
laparoscopy, local and/or systemic MTX administration, bilateral hypogastric
artery ligation, associated with dilatation and evacuation under laparoscopic
guidance, and selective uterine artery embolization (UAE) in combination with
curettage and/or MTX injections.4
Our patient received a systemic injection of MTX (60
mg) and underwent dilatation and curettage. However, because the fetal cardiac
activity was still present, the dose of MTX (60 mg) was repeated on the 4th day
of follow up. This was possible as the patient was hemodynamically stable.
After the second dose of MTX although the serum β-hCG level declined, the
gestational sac continued to increase in size and patient started to feel abdominal
discomfort. So, we performed an ultrasound-guided dilatation and curettage. The
operation was uncomplicated and the patient was discharged from hospital on
postoperative first day.
Rotas et al. in their review of the 112 cases reported
that dilation and curettage was associated with severe maternal morbidity.5
So, several authors recommend MTX, locally or systematically, as first line
therapy for cesarean scar pregnancies.5 This procedure has been
employed with CSP and is successful in 71-80% of cases with no related side
effects.1 In present case we performed systemic MTX prior to surgery
to downgrade trobhoblastic proliferation and decrease to a minimum the risk of
bleeding and uterine rupture as Abadilla et al.6 reported. In
addition Haimov-Kochman et al.7 thought
that gestational sac bulging into uterine cavity after systemic methotrexate
injection is helping to practitioner for an easier and uncomplicated
dilatation-currettage procedure.
Muraji et al.1
reported three cases of CSP that they successfully treated with MTX. In all of
the cases single-dose, systemic MTX was not sufficient, so they had to perform
multiple doses of MTX in two cases, and systemic and local MTX in one case for
to obtain a complete remission.
Wang et al.8 in their study, treated 21 CSP
cases with MTX only, and 50 CSP cases with MTX followed by dilatation and curettage.
The success rates were 76.2% in MTX group and 90.0% in MTX + dilatation and
currettage group, but the difference was not significant. They concluded that
the combined therapy resulted in a shorter time of therapy and indicated a more
favorable effect.
Recently some physicians prefer to use UAE in order to
minimize blood loss. Zhuang et al.9 in
their study compared the efficacy and safety of UAE with systemic MTX for CSP
in 72 patients. They randomly performed UAE to 37 cases and systemic MTX to 35
cases, which all was followed by suction curettage. The primary outpoints include
bleeding loss, serum beta-human chorionic gonadotropin level, and side effects.
They found lower bleeding volumes and hospitalization time in UAE group
compared to MTX group. Besides, there was no severe side effect in both groups.
They concluded that UAE followed by suction curettage appears to have more
advantage and may be a priority option in the treatment of CSP.
Although the treatment of CSP is still controversial,
MTX treatment alone or in conjunction with dilatation-curettage may avoid
unnecessary laparotomy, hysterectomy and preserve fertility.
Consent
Written informed consent was
obtained from the patient for publication of this case report and accompanying
images, and research ethics approval was obtained from the Ethics Committee of
Kahramanmaras Sutcu Imam University. A copy of the written consent is available
for review by the Editor-in-Chief of this journal.
Conflict of interest statement: The authors declare
that they have no conflict of interest.
REFERENCES
1. Muraji M, Mabuchi S,
Hisamoto K, et al. Cesarean scar pregnancies successfully treated with
methotrexate. Acta Obstet Gynecol Scand 2009; 88(6): 720-3.
2. Al-Nazer A, Omar L, Wahba
M, Abbas T, Abdulkarim M. Ectopic intramural pregnancy developing at the site
of a cesarean section scar: a case report. Cases J 2009; 2(11): 9404.
3. Ash A, Smith A, Maxwell D.
Caesarean scar pregnancy. BJOG 2007;114(2):253-63.
4. Tulpin L, Morel O, Malartic
C, Barranger E. Conservative management of a Cesarean scar ectopic pregnancy: a
case report. Cases J 2009; 2(8): 7794.
5. Rotas MA, Haberman S,
Levgur M. Cesarean scar ectopic pregnancies: etiology, diagnosis, and
management. Obstet Gynecol 2006; 107(10): 1373-81.
6. Abadilla ME, Jaspan D,
Dandolu V. Scar pregnancy: a rare complication of caesarean section. Gynecol
Surg 2008; 5(2): 253-5.
7. Haimov-Kochman R,
Sciaky-Tamir Y, Yanai N, Yagel S. Conservative management of two ectopic
pregnancies implanted in previous uterine scars. Ultrasound Obstet Gynecol
2002; 19(4): 616-9.
8. Wang JH, Xu KH, Lin J, Xu JY, Wu RJ. Methotrexate therapy for cesarean section scar
pregnancy with and without suction curettage. Fertil Steril 2009; 92(4):
1208-13.
9. Zhuang Y, Huang L. Uterine
artery embolization compared with methotrexate for the management of pregnancy
implanted within a cesarean scar. Am J Obstet Gynecol 2009; 201(2): 152-3.